What is a Pharmacy Benefit Manager (PBM)?
Adjudicates Claims
Checks Eligibility
Manages Pharmacy Networks
Establishes Formularies
Consolidates Billing
Pays Pharmacy Claims
Reporting
Customer Service
Clinical Programs
Are PBMs and Payers Aligned?
“Relatively few employers believe the goals of their PBMs strongly align with their own goals for managing employee health, productivity and costs.”
National Pharmaceutical Council. (2017). Toward Better Value.
All PBMs are Not Created Equal
“Current PBM models lack transparency
and are overly complicated”
National Pharmaceutical Council. (2017). Toward Better Value.
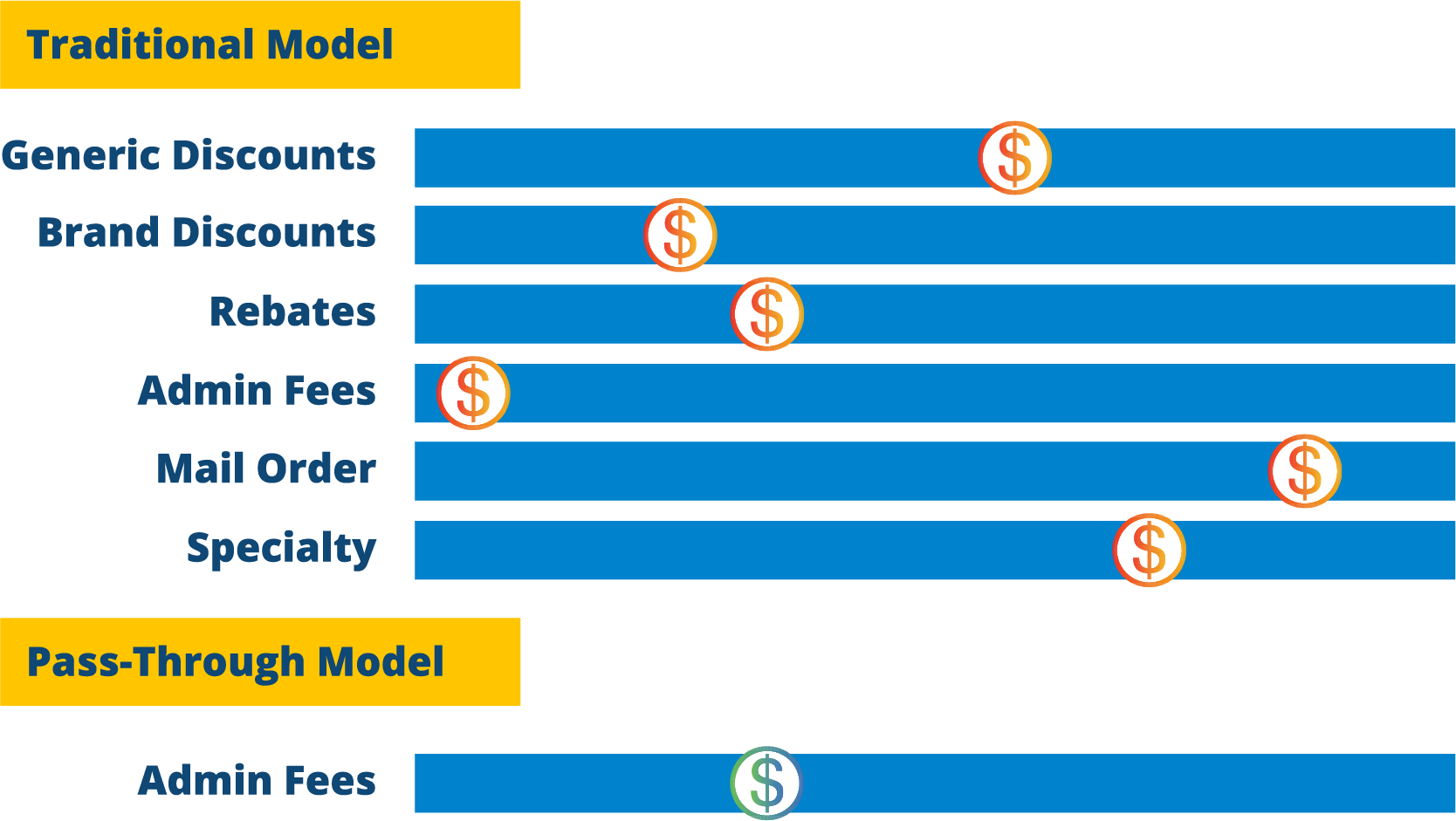
The Foundation of PBMs
Traditional
No Disclosure of Revenue Streams
No Limit to Revenue Streams
Spread Pricing
Transparent Hybrid
Limited Disclosure of Revenue Streams
Varying Limit to Revenue Streams
Partial Pass-Through of Rebates and Pharmacy Pricing to Client
Fully Transparent Pass-Through
Full Disclosure of Revenue Streams
Strict Limit to Revenue Streams (Admin Fee Only)
100% Pass-Through of Rebates and Pharmacy Pricing to Client
 Traditional PBMs retain a network spread, rebates, and other revenues streams as compensation.
Traditional PBMs retain a network spread, rebates, and other revenues streams as compensation.
 Fully Transparent Pass-Through PBMs disclose to the client the exact amount it pays pharmacies. Fully Transparent Pass-Through PBMs are only compensated with an agreed-upon fee for service.
Fully Transparent Pass-Through PBMs disclose to the client the exact amount it pays pharmacies. Fully Transparent Pass-Through PBMs are only compensated with an agreed-upon fee for service.
For every $1,000,000 you are paying your PBM, you are overpaying by $300,000
When Comparing the Traditional PBM model vs. Pass-Through PBM model
How Traditional & Hybrid PBMs
Earn (and Hide) Revenue
1. PBMs do not include all-brand National Drug Code (NDC) for rebate aggregation, resulting in the PBM retaining the NDC rebate rather than the client.
2. PBMs do not pay on Over the Counter (OTC) rebates, although they collect and retain the rebates.
3. PBMs do not pay on insulin rebates, although they collect and retain the rebates.
4. PBMs collect and retain rebates on non-formulary drugs.
5. PBMs do not pay on all diabetes supplies, although they collect and retain stated cost.
6. Differentiating Pre & Post Average Wholesale Price (AWP):
• PBMs pay pharmacies Post-AWP pricing
• PBMs charge clients Pre- AWP pricing, resulting in retainment of Spread
7. PBMs may charge an administrative fee on reversed claims.
8. PBMs adjust the number of drugs available for the guaranteed per prescription rebate by changing the denominator of drugs rebated.
9. PBMs only provide a portion of a point of sale rebates.
10. PBMs utilize multiple Maximum Allowable Cost (MAC) lists:
• One MAC list for the client
• Another MAC list for the pharmacy
11. Direct and Indirect Remuneration (DIR) Fees, also known as a Clawbacks, are revenues collected from the pharmacy 90-days after a paid claim. DIR Fees are 100% retained by the PBM.
12. PBMs collect DIR Fees for not performing Medication Therapy Management (MTM) to the PBMs satisfaction.
13. PBMs are responsible for manipulation of the Most Favored Nation (MFN) pricing.
14. PBMs do not confirm that all pricing will be based on the AWP on the actual date the drug is dispensed, for the actual package size dispensed, and for the actual quantity dispensed.
15. PBMs do not pass-through Usual and Customary (U&C) claims.
16. PBMs take spread on compound claims.
17. PBMs charge the client a professional administration fee for a vaccination, but do not pay the pharmacy the professional administration fee.
18. PBMs may create spread on repackaged NDCs.
19. PBMs negotiate a lower rebate but request a lower acquisition cost for the drug at the in-house pharmacy of the PBM.
20. PBMs negotiate a higher rebate by allowing slimmer early refill rules that increase the chance for an additional fill per year.
21. PBMs dispense 90-day supplies but charge the client for a 100-day supply.
22. PBMs waive copays to steer towards mail order pharmacy.
23. PBMs reclassify generic drugs as a brand drugs, resulting in the PBM paying the pharmacy the generic cost and charging the client the brand cost.
24. PBMs switch the NDC, resulting in the PBM paying the pharmacy the lower cost NDC and charging the client the more expensive NDC.
25. Zero Balance Due: Force shift 100% of patient pay into the contractual guaranteed agreement.
26. PBMs affect the overall effective generic discount by manipulating the following:
27. Reversed/Rejected Claims
28. Compound Claims
29. 340B claims
30. OTC claims NOT covered as part of the plan benefit
31. Devices
32. Vaccines
Misconception of Average Wholesale Price (AWP) Contracting
AWPs have little relevance in projecting final client costs from PBM to PBM. Therefore, the intent of any employer should be to procure medications at the lowest cost per pill.
What will you pay your PBM
for brand and generic drugs?
PBM Profit Levers
Shifting Generic claims into the Brand Category for “inflated savings” Optics
In this example, a traditional PBM moved 2000 claims that processed at AWP-77% into the brand category that has a guarantee of AWP-17%. This falsely gives the client the impression of a successful and competitive contract. Optics are areas within a PBM contract which allow the PBM to create a margin by using angles on contractual words.
In the PBM Optics Generic/Brand chart above, AWP-77% was applied to 2000 extra “Generic” claims which gives the “illusion” of better discounts (AWP-22.5%).
Your PBM is earning revenues if they are, in fact, the ultimate decision maker regarding:
What Drugs Your Members Take
Where the Drugs Come From
How Much They Cost
What if your PBM contractually warrants that their sole source of revenue is the administration fee?
No surprises or hidden tactics. (Yes, such a PBM exists).
Introducing
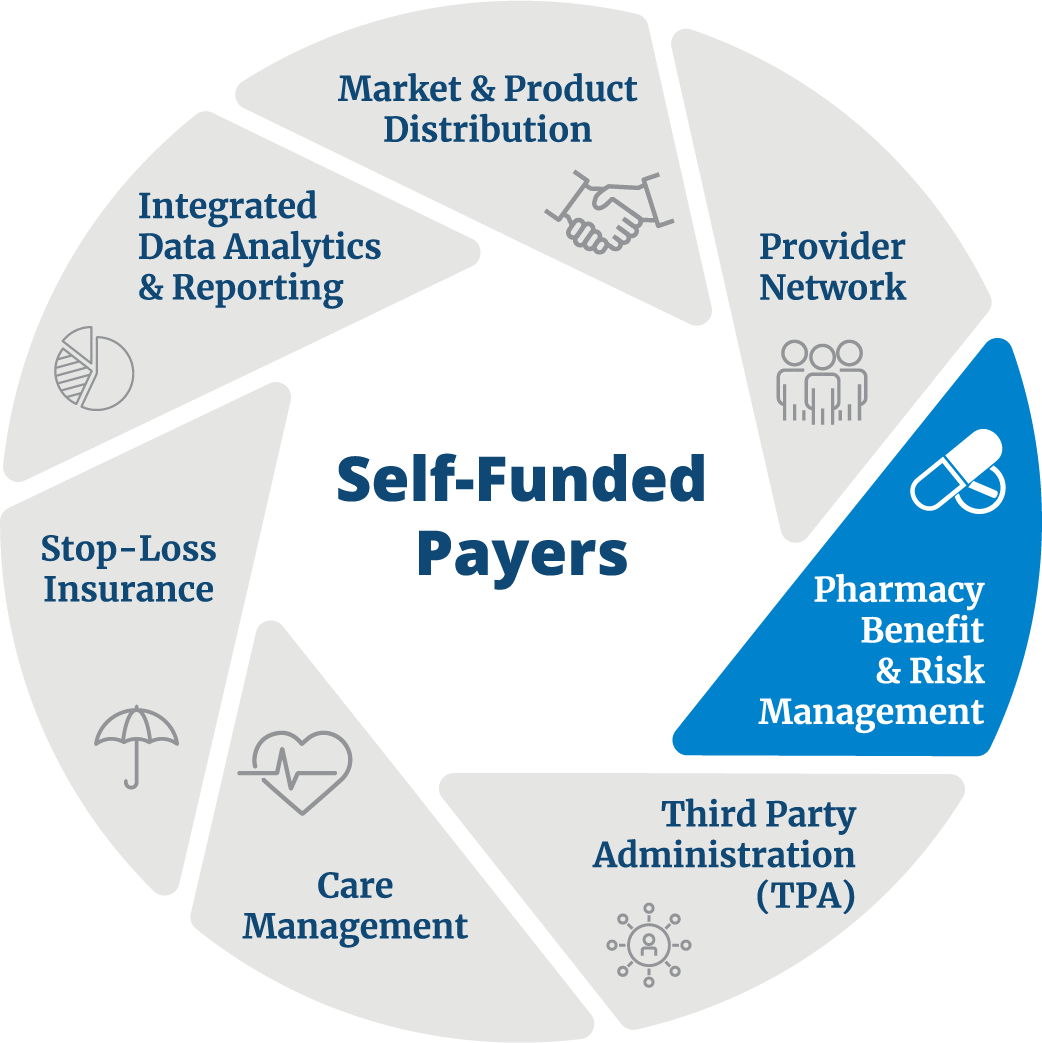
Southern Scripts is a Streamlined, Fully Transparent, and 100% Pass-Through Pharmacy Benefit Manager Dedicated to Self-Insured Plans.
Southern Scripts offers a value-added approach to ensure the employer absolute freedom, control, and choice to their health plan structure without compromising patient experiences and outcomes.
100% Pass-Through Pricing & Rebates
Plan sponsor is charged the exact price the pharmacy is paid
All-Inclusive Administration Fees
No additional fees for prior authorizations, step therapy, reporting, cards, etc.
Pharmacist Driven Management
Unique, targeted clinical utilization strategies
Live, 24/7 Customer Service
Dedicated representatives are available around the clock
Industry Leading Claims Processing Technology
Pioneering the claims processing workflow with cutting-edge technology
Reporting & Data Analytics
Web Portal & Mobile Applications with Quarterly Reporting and Ad Hoc Reporting
Member Tools & Resources
Web Portal & Mobile Applications
Invoicing & Provider Payments
Simple and straightforward accounting services

Southern Scripts is approved by Pharmacists United for Truth and Transparency, a non-profit advocacy organization founded by independent pharmacists and pharmacy owners devoted to exposing the truth about the anti-competitive tactics of pharmacy benefit managers.
“Southern Scripts has been a bright spot in our journey to redefine how healthcare is delivered.”
Supermarket, North America
“Southern Scripts is a completely different PBM – fully transparent and very fair to pharmacies. They are saving plan sponsors millions of dollars, many of which are local municipalities in Louisiana and across the country.”
Pharmacy Owner, Louisiana
“The savings are very real and significant. We have had excellent service and support from Southern Scripts. We have been with Southern Scripts for 18 months and realized our savings in our pharmacy spend was even more than they estimated.”
Medical Center, Arkansas
“It is an understatement to proclaim that Southern Scripts is a saving grace. I can honestly say that they are the one vendor I can count on to run seamlessly, without my intervention, and also engage me and my team periodically with plan insights and options for potential savings strategies.”
H2O Treatment Specialist, Kansas
“There is a great need to move to a Fully Transparent and Pass-Through PBM model and Southern Scripts is my preference. I strongly advise if you are bidding Rx you request a direct quote from Southern Scripts.”
Employee Benefits Brokerage Firm, California
We provide innovative PBM solutions for advisors and plan sponsors. Transform your bottom line today!